Renew Health Blog 💭
Practical Pelvic Floor Thoughts from Your Experts at Renew Health

Navigating Pelvic Organ Prolapse
Navigating Pelvic Organ Prolapse
Pelvic organ prolapse (POP) is a common health challenge that many women face. While it can impact quality of life, understanding POP and learning effective management strategies can help you take control of your pelvic health. In this post, we'll explore what POP is, its symptoms, and practical tips for managing this condition.
What is Pelvic Organ Prolapse?
POP occurs when pelvic organs (like the uterus, bladder, or rectum) descend into the vaginal wall. This happens when the supporting muscles and tissues weaken, often due to childbirth, surgery, or menopause.
Types of Pelvic Organ Prolapse:
Cystocele: Bladder prolapse
Rectocele: Rectal prolapse
Uterine Prolapse: Uterus descends
Enterocele: Small intestine prolapse
Vaginal Vault Prolapse: Top of vagina descends (post-hysterectomy)

Common Symptoms:
Pelvic pressure or fullness
Visible bulge from the vagina
Pelvic discomfort or pain
Urinary or bowel issues
Sexual discomfort
Managing Pelvic Organ Prolapse:
Lifestyle Adjustments
Pressure Management
Use supportive garments or pessaries as recommended
Remember, everyone's experience with POP is unique. Consult your healthcare provider for personalized advice and treatment options. With the right approach, you can effectively manage POP and improve your quality of life.
Patient Success Story
Sarah, a 32-year-old fitness enthusiast and mother of two, came to our clinic four months after the birth of her second child. An avid weightlifter before pregnancy, Sarah was devastated to discover she had developed a stage 2 cystocele (bladder prolapse) postpartum. She experienced a constant feeling of heaviness in her pelvic area and noticed leakage when attempting to return to her beloved squats and deadlifts."I felt like my body had betrayed me," Sarah shared during our initial consultation. "Lifting was my passion, and I was afraid I'd never get back to where I was before pregnancy."We began Sarah's treatment with a comprehensive assessment of her pelvic floor function, core strength, and overall body mechanics. Together, we developed a personalized plan that included:
Pelvic floor rehabilitation exercises (no kegels 😉)
Core strengthening with a focus on proper breathing techniques
Gradual reintroduction of weightlifting with modified techniques
Education on managing intra-abdominal pressure during lifts
Sarah was committed to her recovery, diligently following her home exercise program and attending weekly sessions. We focused on rebuilding her foundation, emphasizing the connection between her breath, core, and pelvic floor. As weeks passed, Sarah's symptoms began to improve. By the two-month mark, she reported a significant reduction in the feeling of heaviness and no longer experienced leakage during light exercises. In the third month, we began to reintroduce heavier lifts, paying close attention to her form and pelvic floor. Sarah was thrilled to find she could perform squats and deadlifts without discomfort or leakage. By the end of our four-month treatment plan, Sarah had not only returned to her pre-pregnancy lifting routine but had surpassed her previous personal bests. She successfully deadlifted 200 pounds and back squatted 185 pounds - both 15 pounds heavier than her pre-pregnancy maxes. "I never thought I'd say this, but I feel stronger now than I did before having kids," Sarah beamed during our final session. "This experience taught me so much about my body and how to lift safely. I'm not just back to where I was - I'm better than ever."
Sarah's story is a testament to the power of dedicated pelvic floor rehabilitation and the importance of a tailored, gradual return to exercise postpartum. Her journey from pelvic organ prolapse to surpassing her pre-pregnancy lifting goals showcases the potential for full recovery and even improvement with proper guidance and commitment.
*patient named changed for privacy, permission given to share
Curious if pelvic floor therapy is right for you? Schedule a free discovery call with our team to learn more about your options. 👇
Give Us A Follow!
Contact Us
Phone: (413) 224-6657
Fax: (413) 273-8203
Email: [email protected]
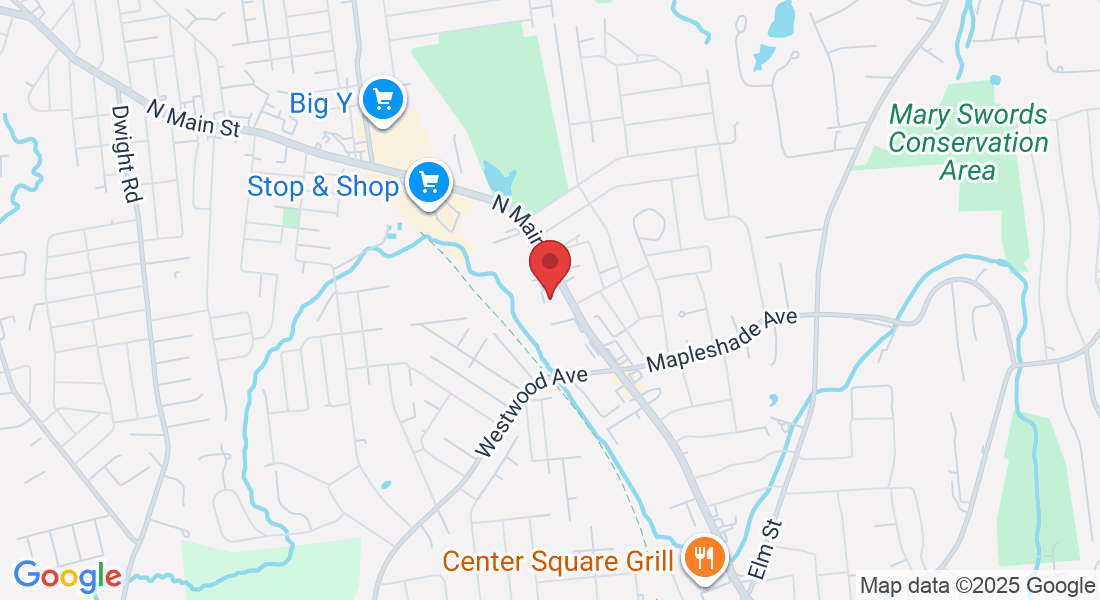
280 N. Main Street Suite 10A, East Longmeadow, MA 01028